Watchful waiting (WW) appeared to be an appropriate approach for patients with basal cell carcinoma (BCC) if they had a limited life expectancy or low-risk BCCs, an observational, real-world cohort study suggested.
In a cohort of 89 patients, watchful waiting was chosen for the treatment of 280 BCCs.
Some 83% of the patients chose watching waiting because of patient-related factors including severe frailty or limited life expectancy, Marieke van Winden, MD, Radboud University Medical Center, Nijmegen, The Netherlands and colleagues reported in JAMA Dermatology.
Fifty-five percent of patients chose tumor-related factors including the absence of symptoms and the indolent nature of the tumor as the reason for choosing watchful waiting while 35% of patients cited the expected treatment burden as the reason why they chose watchful watching instead of treatment right away.
“The main short-term advantage of WW is the avoidance of treatment-related risks and treatment burden,” van Winden and colleagues noted.
“We believe that WW should be discussed with patients and proxies in cases of patients with a limited life expectancy and a relatively low-risk asymptomatic tumor [even though] progression of tumor growth can lead to a substantial tumor burden and most tumors in patients without a limited life expectancy should be considered for active treatment to avoid more extensive tumor and treatment burden,” she added in an email to Breaking Med.
The single-institution study included patients treated at the Radboud University Medical Center in Nijmegen, The Netherlands between January 2018 and November 2020. Patients had a median age of 83 years (interquartile range, (IQR), 73-88 years) and the median follow-up duration of all tumors was 9 months (IQR, 4-15 months).
“The main study outcomes were patients’ reasons for WW…and the proportion and reasons for initiation of later treatment,” the authors explained.
As expected, almost 61% of BCCs were asymptomatic on initial presentation, they noted.
Over the study interval almost half at 46.8% of BCCs increased in tumor size, where the remaining BCCs did not exhibit any tumor growth over time.
Indeed, of those tumors which did not exhibit growth over time, almost one-third decreased in tumor diameter, researchers said.
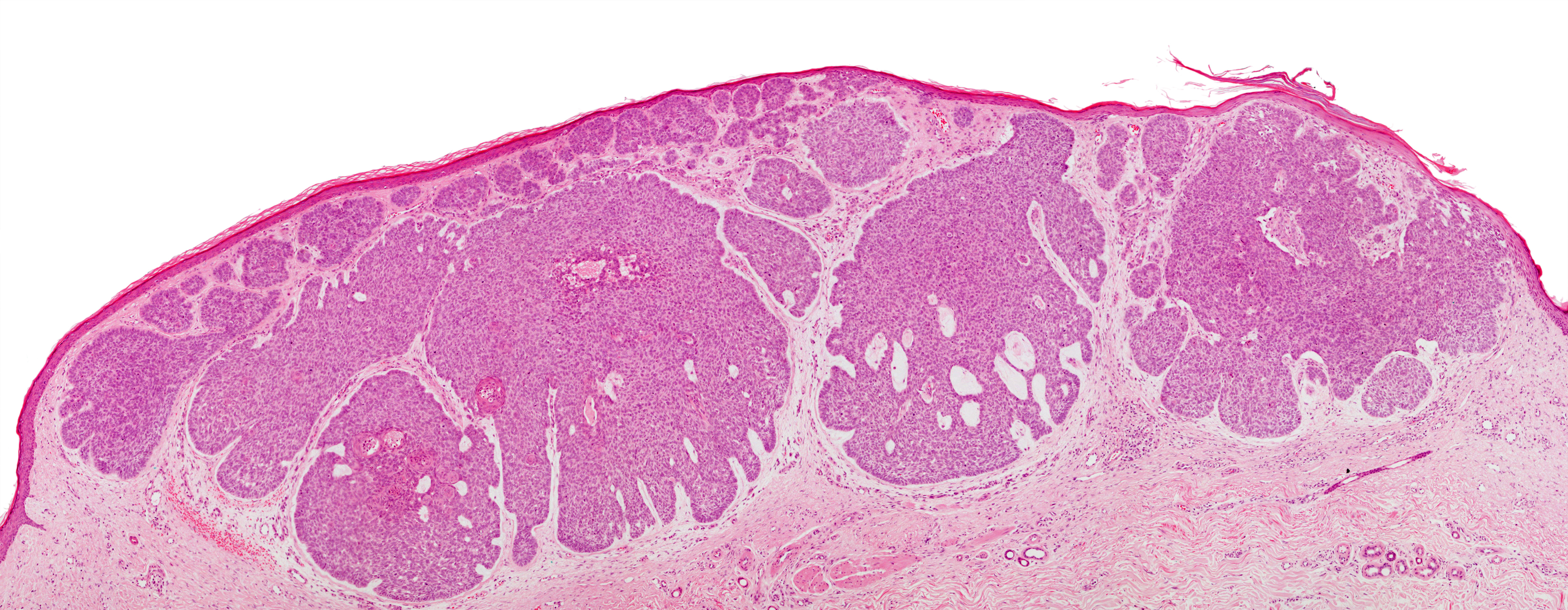
Significantly more low-risk BCCs including nodular, superficial and clinical BCCs remained stable over time or even decreased in diameter.
This was not the case for high-risk BCCs including infiltrative or micronodular BCCs which on multivariable analysis, had over a 3-fold risk of increasing in diameter by over 1 mm over time an Odds Ratio (OR) of 3.35 (95% CI, 1.47-7.96; P=0.005).
In fact, the estimated growth in tumor diameter in one year for high-risk BCCs was 4.46 mm compared to only 1.06 mm increase in diameter for low-risk BCCs, the authors pointed out.
On the other hand, tumor burden should still be considered in patients who have a limited life expectancy with low-risk BCCs, as van Winden noted, as certain tumors on vital locations might need active treatment on short notice.
Furthermore, even in patients who do not have limited life expectancy, “treatment might initially be beneficial as the risk of long-term progression is still unknown and might be significant,” she emphasized.
After initially choosing a watchful waiting approach 63% of patients were treated later, at a median interval of 7 months (IQR, 5-11 months) after their initial presentation, most commonly out of concern for potential tumor burden, as van Winden noted.
Conventional excision was the most frequent treatment approach when patients were eventually treated, the most important reason given by patients for deciding to proceed with treatment being the potential tumor burden.
Of the BCCs for which treatment was eventually performed, more invasive excision was only needed in 2.8% of cases.
“Naturally, we do not advocate a WW approach in each individual patient; the decision for WW should be considered very carefully,” van Winden and colleagues emphasized.
“[However,], it is very important to consider these [patient-related] factors in order to discuss the risk of refraining from treatment in case a patient’s remaining life span exceeds the time to benefit from BCC treatment,” van Winden told BreakingMED in her emailed comments.
For patients who do choose watchful waiting, the authors emphasized that all patients should be followed regularly to determine if watchful waiting is still an appropriate choice, they advised.
Limitations of the study include the fact that the study was observational and retrospective in nature and relied heavily on medical record review. Patients were also not asked a standard set of questions, limiting the amount of data gathered, and there was likely a selection bias in terms of the patients analyzed as the study was done at a university hospital.
Commenting on the findings, Mackenzie Webner, MD, University of Texas MD Anderson Cancer Center, Houston, Texas, pointed out that for the vast majority of patients, BCC has an indolent course and an excellent prognosis with standard excision, Mohs surgery or even topical treatments.
“These treatments are typically well tolerated, but, like any medical intervention, have risks and carry morbidity,” she added.
That said, Webner also stressed that currently, there are no guidelines or recommendations for active surveillance as an evidence-based option for patients with BCCs.
“Unlike many other cancers, BCC is visible on the skin and thus fairly straightforward to monitor for growth and symptoms, which would make it a good candidate for active surveillance,” she wrote.
At the same time, Webner noted that treatments for BCC are fairly straightforward and have relatively low costs, risks and morbidities.
“[T]his does not mean that incorporating active surveillance in the care of BCC is not worthwhile,” she noted. “[However b]efore evidence-based active surveillance in BCC can become a viable option, prospective studies of active surveillance with specified follow-up times and clear outcome measures are needed.”
-
Watchful waiting appeared to be an appropriate treatment course for patients with basal cell carcinoma if they have a limited life expectancy or low-risk BCCs.
-
Low-risk basal cell carcinomas have no to slow growth over time compared to high-risk BCCs.
Pam Harrison, Contributing Writer, BreakingMED™
Neither van Winden nor Webner had any conflicts of interest to declare.
Cat ID: 11
Topic ID: 75,11,282,494,730,11,26,192,255,925