In patients with suspected pulmonary embolism (PE) presenting to the emergency department, combining the YEARS rule with age-adjusted D-dimer threshold in those positive for PERC (the absence of all eight rule-out criteria for PE) was as good as a conventional diagnostic strategy in identifying thrombotic events. Results are published in JAMA.
The YEARS rule—comprised of a diagnostic algorithm that determines the risk of PE—is derived from the Wells score, but unlike this score, YEARS makes use of a variable D-dimer threshold. The conventional diagnostic approach includes subjective estimates of PE probability, D-dimer testing, and chest imaging with computed tomography pulmonary angiography (CTPA) or pulmonary ventilation/perfusion scanning.
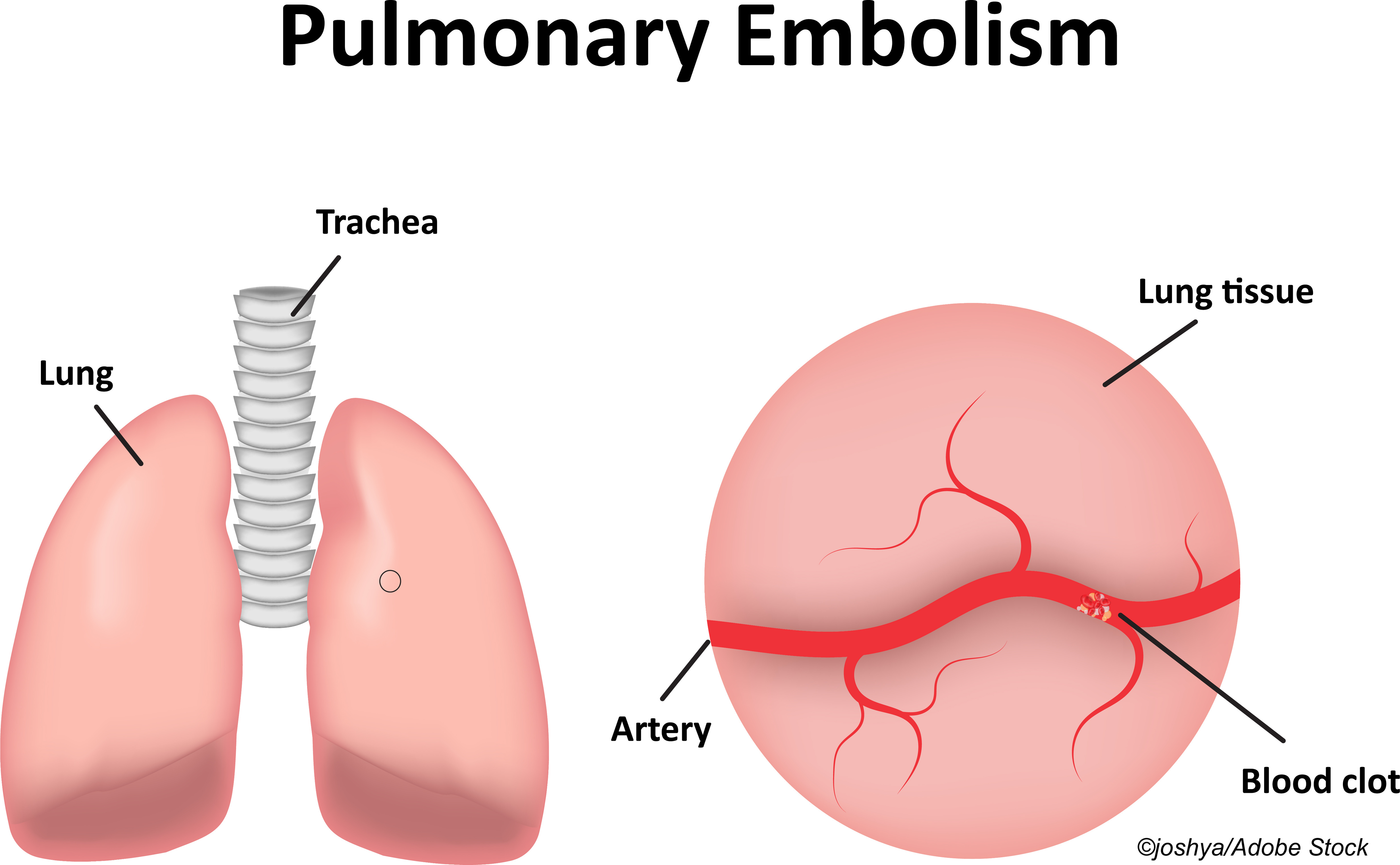
“Because clinical signs of PE and D-dimer testing have low specificity, CTPA is frequently used, with a reported diagnostic yield of only about 10%. CTPA use has increased over the past two decades, resulting in added costs and patient radiation exposure,” according to Yonathan Freund, MD, PhD, of Sorbonne Université, Improving Emergency Care FHU, and the Emergency Department, Hôpital Pitié–Salpêtrière, Assistance Publique–Hôpitaux de Paris, France, and fellow researchers.
“It was reported that the YEARS rule can also safely exclude PE. This rule uses a raised D-dimer cutoff of 1,000 ng/mL (instead of 500 ng/mL) in patients with no YEARS criteria (PE is the most likely diagnosis, clinical sign of deep venous thrombosis, and hemoptysis). However, the YEARS rule has not been investigated in a randomized trial, and its safety when combined with the PERC rule and the age-adjusted D-dimer threshold has not been evaluated,” they noted.
In this cluster-randomized, crossover, non-inferiority trial, Freund and colleagues sought to do this using data from 1,271 patients (mean age: 55 years; 58% female) presenting from October 2019 to June 2020 at 18 emergency departments in France and Spain. The intervention group consisted of 648 patients, and the control group consisted of 623. All had a low clinical risk of PE that was not excluded by the PERC rule, or a subjective clinical intermediate risk of PE, and were followed until October 2020.
“The intervention was a diagnostic strategy to rule out PE that involved both an assessment of the YEARS criteria and D-dimer testing. PE was ruled out in (1) patients with no YEARS criteria and a D-dimer level below the elevated threshold of 1000 ng/mL or (2) patients with one or more YEARS criteria and a D-dimer level below the age-adjusted threshold (age × 10 ng/mL in patients aged ≥50 years). The three YEARS items were assessed by the treating emergency physician. PE was considered as the most likely diagnosis if alternative diagnoses were less likely than PE. A D-dimer level above the relevant threshold triggered chest imaging,” explained researchers.
“During the control period, the diagnostic strategy was based on current recommendations: all patients underwent D-dimer testing with the threshold set at the age-adjusted level. A D-dimer level above the age-adjusted threshold triggered chest imaging,” added Freund and colleagues.
The study’s primary endpoint was venous thromboembolism (VTE) at three months. Freund et al set the noninferiority margin at 1.35%. Secondary endpoints included chest imaging, length of emergency department stay, hospital admission, nonindicated anticoagulation therapy, all-cause death, and all-cause readmission at three months.
A diagnosis of PE was made in the emergency department in 7.1% of patients. At three months, venous thromboembolism was diagnosed in only one patient in the intervention group (0.15%; 95% CI: 0.0%-0.86%) compared with five patients in the control group (0.80% 95% CI: 0.26%-1.86%), for an adjusted difference of the failure rate of −0.64% (1-sided 97.5% CI: −∞ to 0.21%, which was within the preset noninferiority margin of 1.35%).
Freund and colleagues also did a post-hoc analysis of 956 patients with a YEARS score of 0 and found no missed PEs in the intervention group (n=515) compared with three missed PEs in control group (n=441) (failure rates: 0.00% vs 0.68%, respectively). Chest imaging was performed in 22.9% versus 37.2% in the two groups, respectively, for an absolute reduction of 14.3% (95% CI: 8.3%-20.2%).
“In this trial, using PERC, YEARS, and an age-adjusted D-dimer cutoff was associated with lower use of chest imaging compared with a conventional strategy, with the absolute difference between the two groups being 10%,” wrote Freund and fellow researchers.
In their accompanying editorial, Marcel Levi, MD, PhD, and Nick van Es, MD, PhD, both of the Department of Vascular Medicine, Amsterdam Cardiovascular Sciences, Amsterdam University Medical Center, Amsterdam, the Netherlands, commented on these results from Freund et al.
“Taken together, there is a role for efficient diagnostic algorithms to decrease the use of [computed tomography pulmonary angiography] CTPA in patients with clinically suspected pulmonary embolism,” they wrote. “The elegant study by Freund et al shows that this can be achieved by a combination of clinician gestalt, PERC rule, clinical YEARS items, and D-dimer testing with a differential threshold (age-adjusted or fixed high cutoff). However, in the acute clinical setting of emergency medicine, which is usually busy or even hectic, such a rather complex approach toward triage for CTPA is not only time consuming, but may also prove challenging,” they noted.
“A simple diagnostic approach based on the YEARS algorithm combined with age-adjusted D-dimer testing in all patients might have been just as efficient and safe overall, while less burdensome. Further, from a patient perspective, a negative diagnostic algorithm for pulmonary embolism does not diminish the physician’s obligation to consider other diagnoses that explain the symptoms, for which chest CT scans may still be needed and helpful,” concluded Levi and van Es.
Limitations of the study include that randomization was done by center and not patient, protocol deviations in both groups, missing primary outcome information in 37 patients, possibility of exclusion of some eligible patients, and a lack of power to confirm safety in patients with a YEARS score of zero and D-dimer levels above the age-adjusted threshold but below 1,000 ng/mL.
Finally, noted Freund and colleagues, “[T]he subjective criteria of the YEARS score may seem less reliable than a fully structured score, but it has been shown that a subjective assessment of the clinical probability of a PE is reliable.”
-
In ED patients with suspected pulmonary embolism (PE) who were PERC positive, using the YEARS rule combined with the age-adjusted D-dimer threshold was not inferior to identifying thromboembolic events compared with a conventional diagnostic strategy.
-
Using this intervention strategy, the three-month risk of a missed thromboembolic event, compared with a conventional strategy, was 0.15% versus 0.80%.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This research was funded by a grant from the French Health Ministry (Programme Hospitalier de Recherche Clinique 2017). The sponsor was the Assistance Publique–Hôpitaux de Paris.
Freund reported no disclosures.
Levi and van Es reported no disclosures.
Cat ID: 254
Topic ID: 253,254,254,730,914,195,925