1. In this secondary analysis of the RESCUE trial, targeted interleukin 6 (IL-6) ligand inhibition with ziltivekimab was associated with a lower neutrophil-lymphocyte ratio (NLR) at week 12, suggesting it may disrupt atherogenic inflammatory pathways, particularly those mediated by myeloid cell compartment.
2. The estimated treatment difference compared with placebo was -14.6%, -15.3% and -23.6% in the 7.5mg, 15-mg, and 30-mg ziltivekimab treatment groups, respectively.
Evidence Rating Level: 2 (Good)
Study Rundown: The neutrophil-lymphocyte ratio (NLR) has emerged as an inexpensive biomarker that may assess residual inflammatory risk contributing to atherosclerotic disease progression. Ziltivekimab is a novel therapeutic monoclonal antibody that targets the IL-6 ligand. The Trial to Evaluate Reduction in Inflammation in Patients with Advanced Chronic Renal Disease Utilizing Antibody Mediated IL-6 Inhibition (RESCUE) evaluated the effect of ziltivekimab on inflammatory biomarkers in patients at high risk for atherosclerotic disease, including those with chronic kidney disease and elevated high sensitivity C-reactive protein (hsCRP). This secondary analysis aimed to evaluate whether ziltivekimab was associated with a lower NLR compared with a placebo. A total of 264 participants were randomly assigned equally to receive either a placebo, or ziltivekimab 7.5-mg, 15-mg, or 30-mg. The median change in the NLR at 12 weeks was 1.56% in the placebo group, -13.5% in the 7.5-mg group, -14.3% in the 15-mg group, and -22.4% in the 30-mg group. This suggests that ziltivekimab may be associated with multiple proatherogenic inflammatory pathways. Limitations of this study include its modest sample size and brief follow-up period, which did not allow for the assessment of clinical outcomes.
Click to read the study in JAMA Cardiology
Relevant Reading: The neutrophil-lymphocyte ratio and incident atherosclerotic events: analyses from 5 contemporary randomized trials
In-Depth [randomized controlled trial]: This study evaluated whether ziltivekimab was associated with a lower NLR compared with placebo through an exploratory post hoc analysis of the RESCUE trial. This was a double-blind, randomized, placebo-controlled, phase 2 trial conducted between June 2019 to January 2020 with 24 weeks of follow-up. Participants were randomly assigned to receive either a placebo or ziltivekimab 7.5-mg, 15-mg or 30-mg subcutaneously every four weeks. The primary outcome was the change in HLR at 12 weeks. A total of 264 participants (median [IQR] age, 68 [60-75] years; 135 men [51%]; 129 women [49%]) were enrolled. The median (IQR) change in the NLR at 12 weeks was 1.56% (IQR, -15.7% to 20.0%), -13.5% (IQR, -31.6% to 3.20%), -14.3% (IQR, -26.9% to 4.62%), and -22.4% (IQR, -33.3% to -4.27%) in the placebo, 7.5 mg, 15 mg, and 30 mg groups respectively. The estimated treatment difference compared with placebo was -14.6% (95% CI, -24.8% to -4.81%; P = .004), -15.3% (95% CI, -25.2% to -5.10%; P = .004), and -23.6% (95% CI, -33.2% to -14.2%; P < .001) in the 7.5-mg, 15-mg, and 30-mg groups, respectively. A similar reduction in the ANC was observed in the same groups.
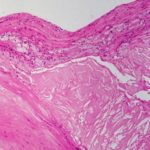
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.