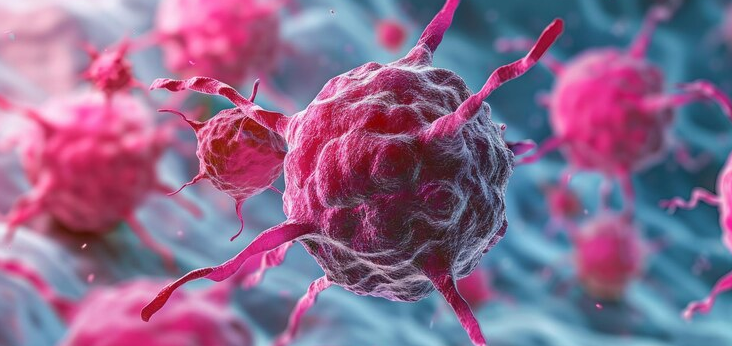
The following is a summary of “Interplay of inflammatory markers and anti-SARS-CoV-2 antibodies in COVID-19 mortality: A prospective cohort study,” published in the April 2024 issue of Infectious Disease by Mink et al.
Researchers conducted a retrospective study exploring the combined effects of vaccination, pre-existing anti-SARS-CoV-2 antibodies, and inflammation on immune response and mortality in patients with COVID-19.
They involved 1,031 hospitalized patients with COVID-19 from five hospitals. Anti-SARS-CoV-2-spike antibodies, interleukin-6 (IL6), and CRP levels were assessed upon hospital admission. The predefined outcome was all-cause in-hospital mortality.
The results showed lower CRP and IL6 in patients with antibody levels exceeding 1200 BAU/ml (P<0.001). Patients with high CRP (>6 mg/dl) or IL6 (>100 pg/ml) along with low antibody levels (<1200 BAU/ml) had an approximately 8-fold increased mortality risk compared to patients with low inflammation and high antibodies (CRP: aHR 7.973, 95% CI 2.744-23.169, P<0.001; IL6: aHR 8.973, 95% CI 3.549-22.688, P<0.001).
Investigators concluded that hospitalized patients with COVID-19 with low antibody levels and high inflammatory markers had the highest mortality rates.
Source: sciencedirect.com/science/article/pii/S1201971224000870