A full one-fifth of patients treated with chimeric antigen receptor T-cell (CAR-T) therapy experienced adverse cardiovascular and pulmonary events (CPAEs), which include tachyarrhythmias, cardiomyopathy, pericardial and pleural disorders, and venous thromboembolism (VTE), according to a recent study published in the Journal of the American College of Cardiology.
Further, most patients (68.3%) experienced overlapping CPAEs and cytokine release syndrome (CRS), which increased their risk of fatality.
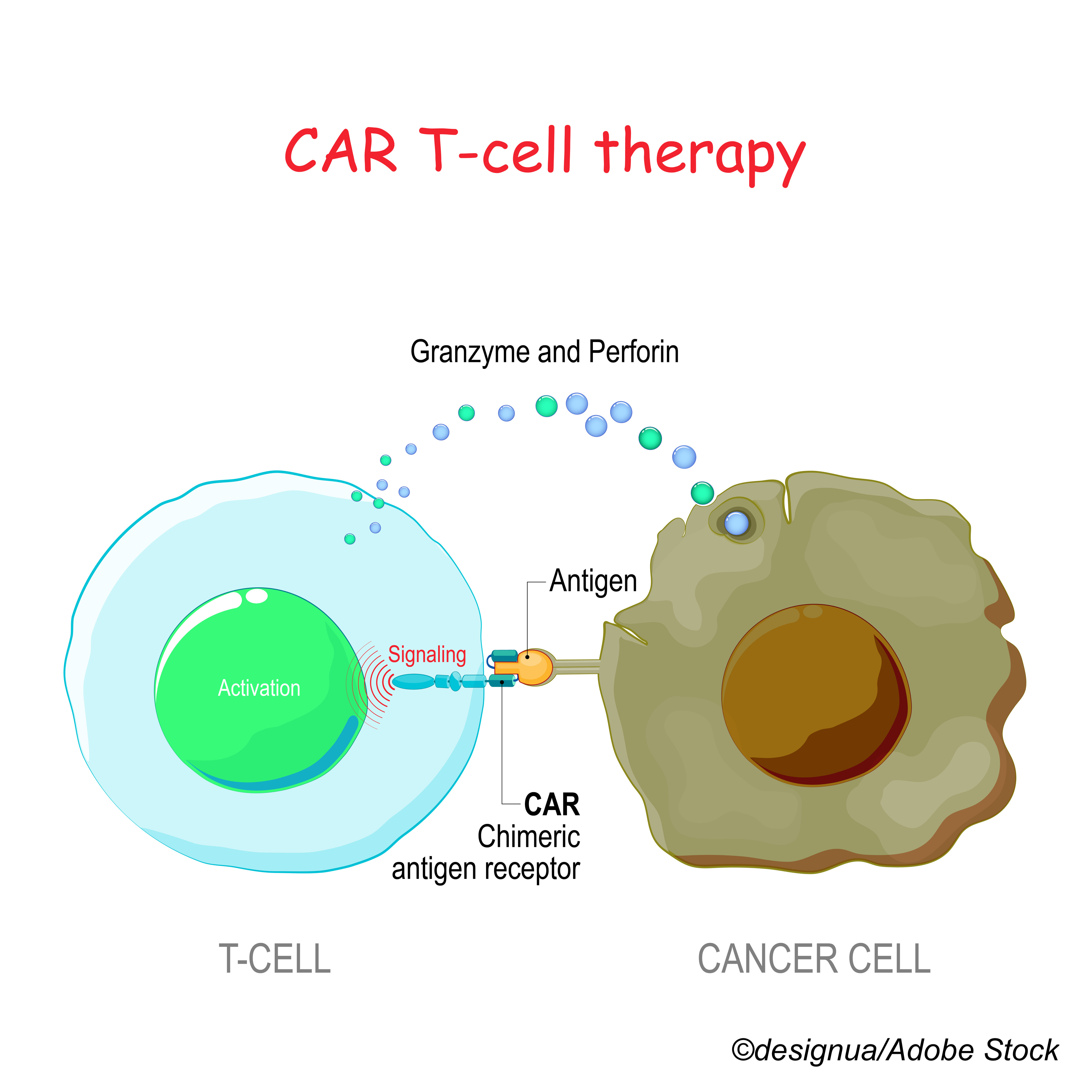
“Chimeric antigen receptor T cells (CAR-T) are genetically engineered T-cells that have transformed the care of patients with hematological malignancies. Pivotal phase II trials demonstrating high-response rates in treatment-resistant hematological malignancies have led to FDA approval of several CAR-T products for B-acute lymphoblastic leukemia and large B-cell lymphoma. More recently, CAR-T therapy has been approved for additional indications, including follicular lymphoma, mantle cell lymphoma, and multiple myeloma,” senior author Roni Shouval, MD, of Memorial Sloan Kettering Cancer Center, New York, told BreakingMED.
“Clinical trials have reported low rates of cardiovascular adverse events after CAR-T therapy. However, populations with significant cardiac comorbidities were excluded. Furthermore, studies may have been underpowered to address this sort of question. Retrospective analyses suggest non-negligible cardiotoxicity after CAR-T, but cohorts were generally small. Therefore, we were interested in a comprehensive assessment of cardiovascular and pulmonary adverse events in a large number of patients reported in the FDA Adverse Event Reporting System (FAERS) database,” he added.
Using data from the FAERS database—which includes voluntary reporting from health care professionals and consumers and required reporting by manufacturers—Shouval and colleagues identified 2,657 patients treated with an approved CAR-T therapy from July 1, 2014, to June 30, 2020. Of these, 65.2% received axicabtagene-ciloleucel and 34.8% received tisagenlecleucel. Most patients were treated for non-Hodgkin lymphoma (83.7%), and 14.4% had B-cell acute lymphoblastic leukemia (B-ALL) and were treated with tisagenlecleucel.
In all, 54.8% of CAR-T recipient safety reports included CRS, and 20.5% included CPAEs, among whom 68.3% reported concurrent CRS. Researchers noted that all CPAEs were positively correlated with CRS, with weaker correlations between hypotension and other CPAEs.
Compared with the full database of over 7 million patients, those receiving CAR-T treatments had a significantly increased reporting of the following CPAEs:
- Hypotension: 10.8% (adjusted reporting odds ration [adj ROR]: 13.43; 95% CI: 1078-16.73).
- Cardiomyopathy: 2.6% (adj ROR: 3.51; 95% CI: 2.42-5.09).
- Tachyarrhythmias: 2.8% (adj ROR: 2.78; 95% CI: 2.21-3.51).
- Pericardial diseases: 0.4% (adj ROR: 2.26; 95% CI: 1.25-4.09).
- Cardiogenic shock: 1.8% (adj ROR: 1.99; 95% CI: 1.50-2.64).
- Respiratory failure: 2.7% (adj ROR: 6.01; 95% CI: 4.28-8.44).
- Pleural disorders: 1.7% (adj ROR: 3.91; 95% CI: 2.92-5.23).
Shouval et al also compared CAR-T products and found higher reports of the following events in patients treated with axicabtagene-ciloleucel:
- Cytokine release syndrome (CRS): 59.1% versus 46.9%, respectively (adj. ROR: 1.40; 95% CI: 1.04-1.90).
- Tachyarrhythmias: 34.4% versus 1.7% (adj. ROR: 1.82; 95% CI: 1.04-3.18).
- Venous thromboembolic events (VTE): 1.6% versus 0.7% (adj. ROR: 2.86; 95% CI: 1.18-6.93).
Reports of composite severe cardiovascular advents were similar between groups.
When researchers assessed specific terms cited in some CPAE categories, they found that within reports of cardiomyopathy, cardiorenal syndrome was common (34.8%), and tachyarrhythmias included atrial fibrillation (74.3%) and ventricular arrhythmias (18.9%), which were only associated with axicabtagene-ciloleucel.
Nonmalignant effusions comprised the majority of pleural (89.1%) and pericardial disorders (100%), while deep vein thrombosis (55.9%) and pulmonary embolism (35.3%) comprised the majority of events categorized as VTE.
The median time from infusion to CPAE was 0 to 2 days, and most CPAEs were reported within the first 10 days after infusion. Patients experiencing VTEs and cardiogenic shock had later peaks, however, before post-infusion day 30.
The fatality rate of CPAEs was 30.9%, and the rate for CRS was 17.4%. The highest fatality rates occurred with cardiogenic shock (80.9%) and respiratory failure (66.2%). Fatality rates ranged between 27.3%-40.5% for pericardial diseases, VTEs, tachyarrhythmias, cardiomyopathy, and pleural disorders.
Patients treated with axicabtagene-ciloleucel with high cardiovascular risk were overrepresented compared with the whole cohort (77.9% versus 64.1%, respectively; P˂0.001). Patients at high cardiovascular risk experienced CPAEs more often compared with those not at risk (38.0% versus 19.1%, respectively; P˂0.001), but CRS rates were comparable (60.1% versus 54.4%; P=0.13).
“Our data suggest that cardiovascular adverse events following CAR-T therapy are more common than initially thought and potentially lethal. While the true incidence of cardiovascular complications cannot be directly deduced from FAERS, we estimate that over 10% of patients experience them. Furthermore, patients with cardiovascular risk factors are at higher risk for developing significant cardiotoxicity,” Shouval told BreakingMED.
Were these results surprising? According to Shouval, “We expected to find a strong correlation between cardiovascular adverse events and cytokine release syndrome (CRS). CRS is an acute systemic inflammatory process manifesting with fever and organ dysfunction following CAR-T therapy. However, some cardiovascular adverse event reports were not concomitant with CRS, suggesting that cardiotoxicity is not merely an epiphenomenon of CRS. Clearly, more research is needed to understand better the mechanism contributing to cardiac injury in patients receiving CAR-T.”
Should clinicians screen patients for cardiovascular risk factors before initiating CAR-T therapies?
“Given the relatively high reported mortality associated with cardiovascular adverse events in this population, I believe there is room for optimizing screen of cardiovascular risk factors and optimizing their management before administration of the CAR-T cells. Furthermore, in patients with cardiovascular morbidity developing CRS, aggressive management, with early introduction of anti-inflammatory therapy should likely be employed. IL6 is a driver of CRS and inhibiting it using agents such as tocilizumab may improve patient outcomes,” Shouval said.
In their accompanying editorial, Ana Barac, MD, PhD, of the National Heart, Lung, and Blood Institute, National Institutes of Health, and Elad Sharon, MD, MPH, of the National Cancer Institute, Bethesda, Maryland, wrote:
“Chimeric antigen receptor T cells (CAR-Ts) are a novel class of immunotherapeutic agents that exhibit their cytotoxic antitumor effect using the genetic engineering of T cells. In addition to immune-related adverse events (irAEs), known to occur with immune checkpoint inhibitors, CAR-T therapies have also been associated with novel forms of toxicities. The most recognized is the cytokine release syndrome (CRS) (reported in the range of 55% to 90% of patients in clinical CAR-T trials), which may present with fever and nausea, capillary leak syndrome, hypotension, and tachycardia.”
They applauded the authors for a well-done study, but they noted: “The true incidence of CPAEs remains unknown because of the wide range of factors influencing voluntary reporting (eg, severity of treated disease, expected complications, perceived benefit versus risk, marketing, and other trends) and the lack of knowledge about the accurate number of patients exposed to CAR-T treatment. Therefore, a higher ROR does not equate to a higher individual patient risk, but rather represents an extent of reporting itself. Similarly, the results of the ROR comparisons between the 2 approved CAR-T agents, axicabtagene-ciloleucel and tisagenlecleucel, although plausible, remain hypothesis-generating. To diagnose, predict, and identify specific treatments for CVAEs associated with CAR-T therapies, we will need much more.”
“This report joins an increasing number of postmarketing safety analyses, particularly in the area of irAEs, which identify relevant CV safety signals that might have not been captured in clinical trials,” concluded Barac and Sharon.
Limitations of the study include the inability to determine the incidence of CPAEs after CAR-T therapy because the number of patients exposed to the drugs was unknown; limited granular data on patient, disease, and treatment features; confounding by age in patients with B-ALL treated with tisagenlecleucel (only approved for patients up to 25 years old).
-
After chimeric antigen receptor T-cell (CAR-T) therapy, a full one-fifth of patients experienced adverse cardiovascular and pulmonary events (CPAEs).
-
Most patients (68.3%) experienced overlapping CPAEs and cytokine release syndrome (CRS), which increased their risk of fatality.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was funded in part by grants from the NIH/NCI Cancer Center and the NIH/NCI.
Shouval had no disclosures.
Barac and Sharon had no disclosures.
Cat ID: 116
Topic ID: 78,116,730,914,116,935,192,195,925



Create Post
Twitter/X Preview
Logout