Ponesimod outperformed teriflunomide on nearly all fronts for managing annualized relapse rate (ARR), fatigue, magnetic resonance imaging activity, brain volume loss, and disease activity in patients with relapsing multiple sclerosis (RMS), according to results from the phase III OPTIMUM trial.
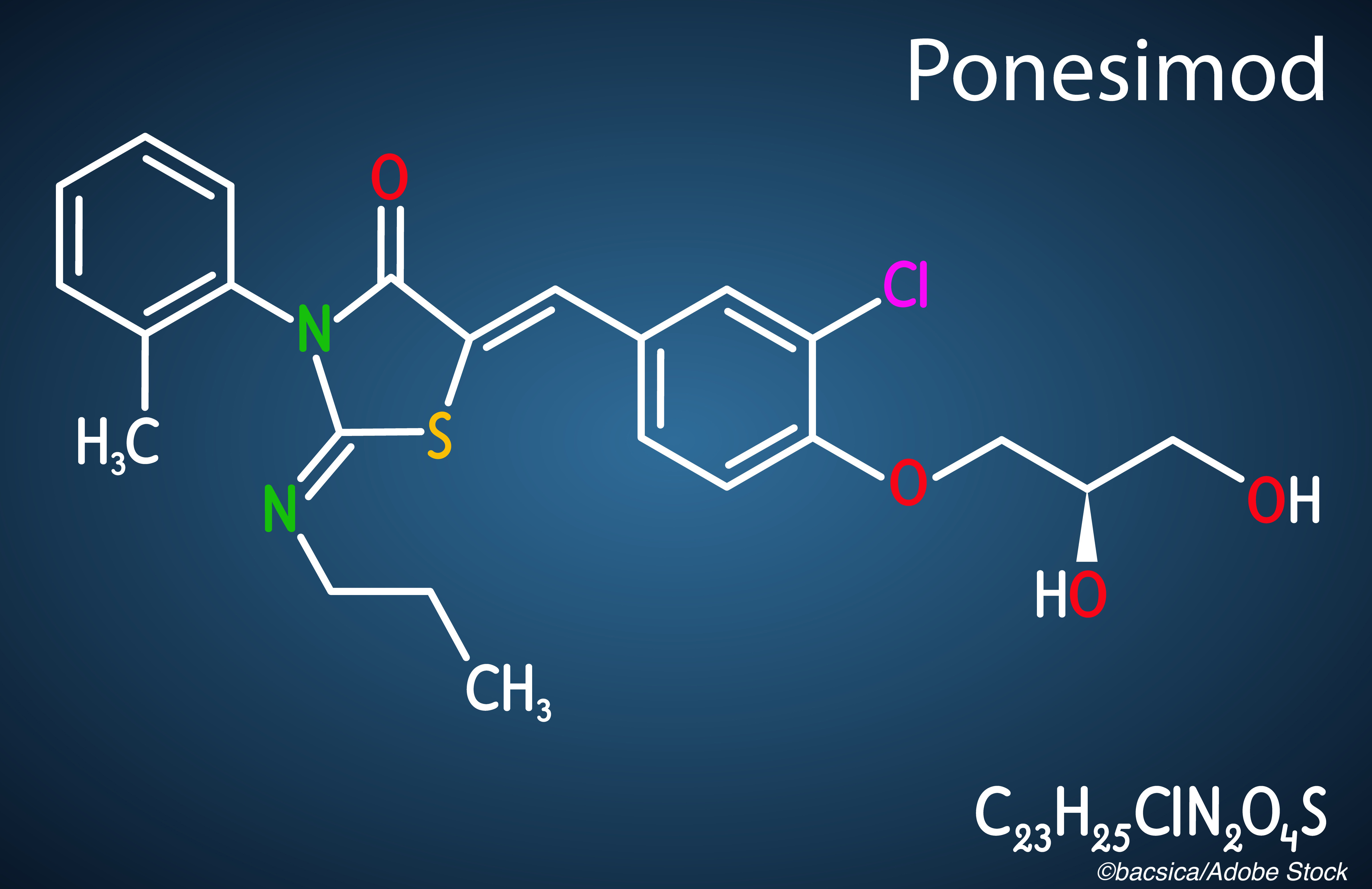
The only trial measure in which ponesimod — a selective sphingosine-1-phosphate receptor 1 (S1P1) modulator — did not best the comparator drug was in reducing confirmed disability accumulation, for which the difference was not statistically significant, Ludwig Kappos, MD, of the Departments of Medicine, Clinical Research, Biomedicine, and Biomedical Engineering at University Hospital and University of Basel in Basel, Switzerland, and colleagues reported in JAMA Neurology. This trial formed the basis of the FDA’s March 19 approval of ponesimod for adults with RMS.
“Ponesimod was superior to teriflunomide, an oral pyrimidine synthesis inhibitor approved for the treatment of MS, on the primary study outcome, reduction of ARR (by −30.5%),” Kappos and colleagues wrote. “Superiority versus teriflunomide was also shown in the analysis of two key secondary outcomes: the reduction of CUAL, an established MRI measure of focal inflammatory disease activity (−56%), and improvement of MS-associated fatigue, as measured with the FSIQ-RMS weekly symptom score (mean difference, −3.57). Despite the well-known negative implications on quality of life and the high socioeconomic burden associated with fatigue, no previous phase III study in MS has addressed fatigue prospectively as a key outcome.”
To their knowledge, the OPTIMUM trial was the first phase III study to compare the efficacy and safety of two oral disease-modifying therapies (DMTs) in RMS, the study authors added.
For this multicenter, double-blind, active-comparator, superiority randomized clinical trial, Kappos and colleagues evaluated the efficacy, safety, and tolerability of 20 mg of ponesimod (up-titrated from a 2 mg starting dose for the first 14 days to reduce first-dose cardiac effects of S1P1 modulators) against 14 mg of teriflunomide for 108 weeks in patients with RMS. The study was conducted from April 2015-May 2019 in 162 centers across 28 countries in North America, Europe, Mexico, Israel, and Turkey — patients were stratified by use of MS DMTs in the last 2 years prior to randomization and baseline Expanded Disability Status Scale (EDSS) score (≤3.5 or >3.5).
The OPTIMUM trial cohort consisted of adult patients ages 18-55 years with RMS, an EDSS score between 0 and 5.5, and recent clinical or magnetic resonance imaging (MRI) activity. A total of 1,468 patients were screened, 1,133 of whom were randomized 1:1 to either ponesimod (n=567) or teriflunomide (n=566) — the median age was 37.0, and 735 (64.9%) were women. Two randomized patients in the ponesimod group did not receive the study treatment, leading to a total cohort of 1,131 for the final analysis.
The study’s primary endpoint was ARR; secondary end points included changes in symptom domain of Fatigue Symptom and Impact Questionnaire-Relapsing Multiple Sclerosis (FSIQ-RMS) at week 108, the number of combined unique active lesions per year on MRI, and time to 12-week and 24-week confirmed disability accumulation. Exploratory end points included percentage change in brain volume and no evidence of disease activity (NEDA-3 and NEDA-4) status.
At 108 weeks, “ponesimod reduced ARR by 30.5% compared with teriflunomide (mean ARR, 0.202 vs 0.290; rate ratio, 0.695 [99% confidence limits (CLs), 0.536-0.902]; P<0.001,” the study authors found. Ponesimod also led to improved fatigue symptoms (mean difference −3.57 [−0.01 versus 3.56; P<0.001]) and reduced combined unique active lesions per year (56% [1.405 versus 3.164; P<0.001]) — confirmed disability accumulation was no different between the ponesimod and teriflunomide groups at 12 (10.1% versus 12.4%; hazard ratio, 0.83; P=0.29) and 24 weeks (8.1% versus 9.9%; hazard ratio, 0.84; P=0.37).
As for the exploratory outcomes, in the ponesimod group, “brain volume loss at week 108 was lower by 0.34% (–0.91% versus –1.25%; P<0.001); the odds ratio for NEDA-3 achievement was 1.70 (25.0% versus 16.4%; P<0.001),” Kappos and colleagues added. “Incidence of treatment-emergent adverse events (502 of 565 [88.8%] vs 499 of 566 [88.2%]) and serious treatment-emergent adverse events (49 [8.7%] versus 46 [8.1%]) was similar for both groups. Treatment discontinuations because of adverse events was more common in the ponesimod group (49 of 565 [8.7%] versus 34 of 566 [6.0%]).”
The most common treatment-emergent adverse events were increased alanine aminotransferase levels (110 [19.5%] versus 53 [9.4%]), nasopharyngitis (109 [19.3%] versus 95 [16.8%]), headache (65 [11.5%] versus 72 [12.7%]), upper respiratory tract infection (60 [10.6%] versus 59 [10.4%]), and alopecia (18 [3.2%] versus 72 [12.7%]) in the ponesimod and teriflunomide groups, respectively. And, Kappos and colleagues pointed out, while most treatment discontinuations in the ponesimod group were due to adverse events, more patients in the teriflunomide group discontinued treatment due to lack of efficacy, “consistent with the greater benefit of ponesimod observed across multiple efficacy end points.”
Kappos and colleagues noted that, when taken together, “the effect of ponesimod on fatigue and the reduction of brain volume loss, shown against a drug with an established effect on brain volume loss, suggests that ponesimod’s benefits are not restricted to suppressing relapses and focal lesions reflecting short-term events in the pathogenesis of MS but extend to the prevention of tissue damage accumulation.”
As for the lack of a statistically significant difference for 12-week confirmed disability discontinuation, the authors noted that the study cohort’s baseline EDSS scores (mean, 2.6) and the proportion of patients with EDSS scores of 3.5 or less (83.5%) indicated a relatively low level of disability among the study participants. This, coupled with the relatively low rate of confirmed disability accumulation events observed in the two study groups, may have limited the study’s ability to detect significance differences between the ponesimod and teriflunomide groups.
- Ponesimod proved superior to teriflunomide for improving annualized relapse rate, fatigue, magnetic resonance imaging activity, brain volume loss, and disease activity status in patients with relapsing multiple sclerosis (RMS).
- Results from the phase III OPTIMUM trial led to the FDA approval of ponesimod for RMS in March 2021.
John McKenna, Associate Editor, BreakingMED™
Funding was provided by Janssen Research & Development LLC, and the OPTIMUM study was supported by Actelion Pharmaceuticals, part of Janssen Pharmaceutical Companies.
In the last three years, Kappos’ institution received steering committee, advisory board, consultancy fees, and/or support for educational activities exclusively for research support from Actelion Pharmaceuticals, as well as Allergan, Bayer Healthcare, Biogen, Merck, Novartis, Pfizer, Roche, and others. Study coauthors Burcklen, Hennessy, Linscheid, Pirozek-Lawniczek, Vaclavkova, Kracker, and Sherz are employees of Actelion. Several coauthors hold stock in Actelion and Johnson & Johnson.
Cat ID: 36
Topic ID: 82,36,730,36,192,925