Thomas Powles, M, of Barts Cancer Institute, Queen Mary University of London, and his co-investigators also published their findings in The New England Journal of Medicine .
“Overall survival at 1 year was 71.3% in the avelumab group and 58.4% in the control group (median overall survival, 21.4 months versus 14.3 months; hazard ratio for death, 0.69; 95% confidence interval [CI], 0.56 to 0.86; P = 0.001),” they wrote.
The researchers noted that although platinum-based therapy is the current standard — about half of patients have an objective response — “most patients have disease progression within 9 months, and the median overall survival is 14-15 months with cisplatin-based regimens and 9 to 10 months with carboplatin-based regimens among patients who are not suitable candidates for cisplatin-based therapy.”
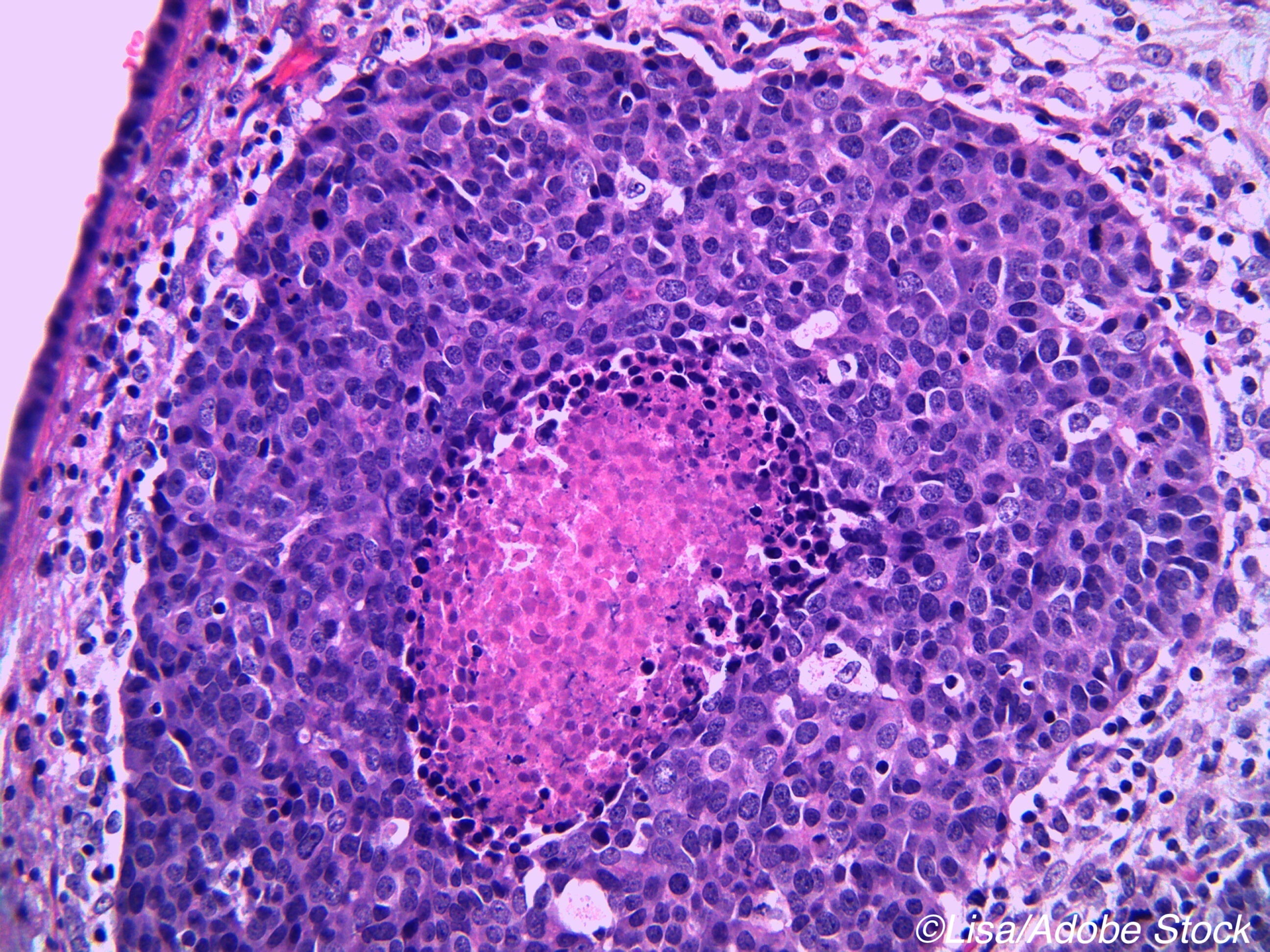
Urothelial carcinoma does, however, have a number of features or characteristics that are known to increase response to immune checkpoint inhibitors.
“Avelumab is an anti–PD-L1 antibody that has been approved in several countries for the treatment of locally advanced or metastatic urothelial carcinoma after disease progression during or after platinum-containing chemotherapy, on the basis of results from a large, phase 1b cohort (involving 242 patients) in which an objective response was observed in 16.5% of the patients and the overall survival at 2 years was 20.1%,” Powles and colleagues wrote. “We hypothesized that avelumab maintenance therapy would improve outcomes in patients who had received first-line platinum-based chemotherapy for advanced urothelial carcinoma.”
They enrolled 700 patients at 197 sites in 29 countries, randomly assigning them to avelumab (n=350) on top of best supportive care or best supportive care without avelumab (n=350). A little more than half of the patients (358) had PD-L1-positive tumors: 189 of then were in the avelumab group and 169 in the control group. The primary efficacy endpoint was overall survival and the secondary endpoint were progression-free survival.
Among the findings:
- Median overall survival for persons with PD-L1-negative tumors was 18.8 months in the avelumab arm and 13.7 months in the control arm.
- Median progression-free survival was 3.7 months in avelumab arm versus 2.0 months in the control arm.
- Among patients with PD-L1-positive tumors the median progression-free survival was 5.7 month in the avelumab arm versus 2.1 months in the control group.
- Among patients with PD-L1 negative tumors the median progression-free survival was 3.0 months in the avelumab arm versus 1.9 months in the control group.
Serious adverse events — grade 3 or higher — occurred in 163 avelumab-treated patients and 41 patients discontinued treatment due to AEs, while 87 control group patients experienced serious adverse events.
“Death was attributed by the investigator to the toxicity of trial treatment in two patients (0.6%) in the avelumab group. One patient had sepsis after a urinary tract infection and possible central venous catheter infection after receiving 11 infusions of avelumab. The other patient had an ischemic stroke 100 days after receiving a single dose of avelumab and after disease progression and adverse events of limb venous thrombosis, pulmonary embolism, and acute myocardial infarction,” they wrote.
The authors noted that the overall survival benefit was longer with avelumab “despite the more frequent use of subsequent treatment in the control group (in 61.7% of patients), including immune checkpoint inhibitors (in 43.7%), a finding that highlights the benefit of starting avelumab immediately after first-line chemotherapy instead of waiting for disease progression. Furthermore, separation of the overall survival curves and the progression-free survival curves in favor of avelumab occurred early in the course of treatment and was maintained, which suggests that so-called hyperprogression (a potential and unexpected deleterious effect of treatment with a checkpoint inhibitor in which tumors would paradoxically progress faster than if they were untreated) did not occur with avelumab maintenance therapy in patients with advanced urothelial cancer.”
The findings, the authors concluded, support first-line maintenance with avelumab, rather than waiting for disease progression.
-
The findings from this randomized trial of 700 patients with advanced urothelial cancer suggest that avelumab maintenance therapy improves overall survival.
-
Note that in this trial, patients benefited from avelumab therapy regardless of PD-L1 status; however, those with PD-L1 positive tumors achieved a greater benefit.
Peggy Peck, Editor-in-Chief, BreakingMED™
Powles reported grant support or consultant fees from Astellas Pharma, AztraZeneca, Bristol-Myers Squibb, Eisai, EMD Serono Inc., Exelxis, Progenics, Roche Laboratories, Sanofi US Services, Inc., Seattle Genetics, Tyme Inc., and UroGenPharma.
Cat ID: 120
Topic ID: 78,120,730,120,697,935,192,241,925,696



Create Post
Twitter/X Preview
Logout