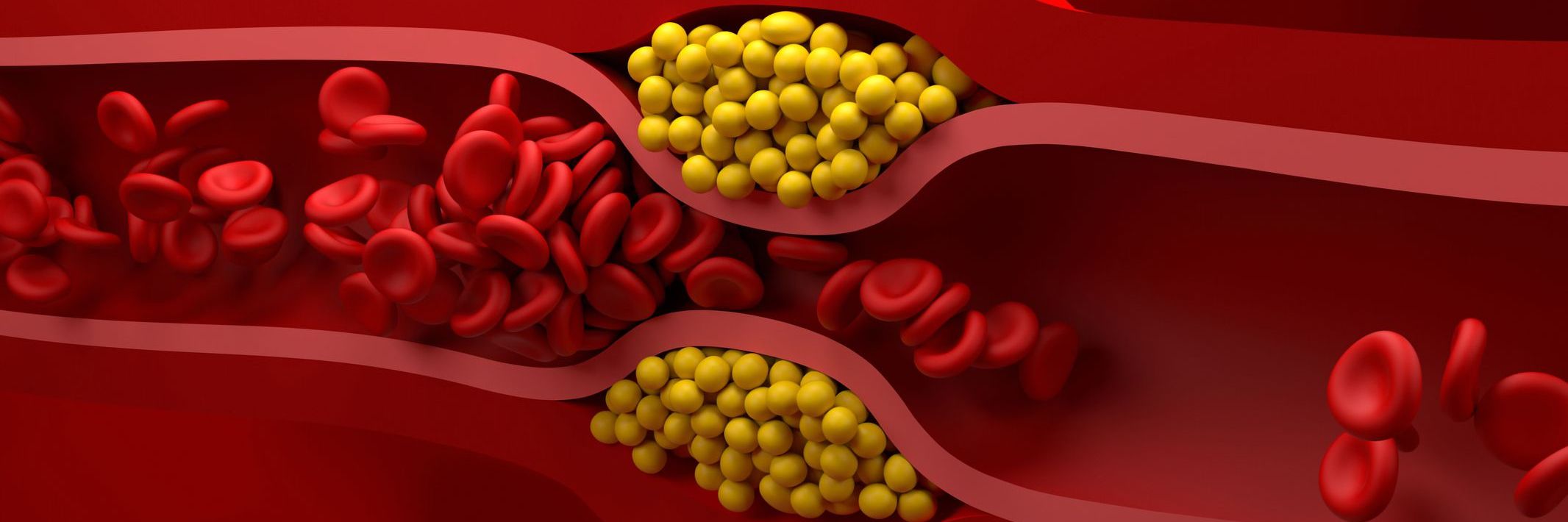
Guidelines developed by the American College of Cardiology/American Heart Association (ACC/AHA) recommend lipid-lowering therapies (LLTs) to reduce low-density lipoprotein cholesterol (LDL-C) and atherosclerotic cardiovascular disease (ASCVD) risk. This study described LLT utilization patterns and LDL-C goal achievement (to <70 mg/dL) among patients with ASCVD in the US.
This retrospective study was conducted using Optum’s de-identified Clinformatics® Data Mart Database (CDM). Patients with their first ASCVD diagnosis (index date) in the CDM database between July 1, 2015, and December 31, 2018, were followed for ≥12 months to assess LLT utilization patterns and change in LDL-C. LLTs included were statins and non-statin LLTs (ezetimibe, fibrates, and proprotein convertase subtilisin/kexin type 9 inhibitors). Adherence was measured as the proportion of days covered (PDC), defined as the number of days with drug on-hand (or number of days exposed to drug) divided by the 12-month follow-up period. Patients with PDC ≥0.8 were considered adherent.
Among the patients with ASCVD (N = 1,424,893) included in this study, only 621,978 (43.7%) had at least one LDL-C measurement at baseline (6 months prior to and 3 months after the index date). The mean age was 71.5 years, and almost half of the patients were female. Patients were followed for a mean (standard deviation [SD]) duration of 30.6 (11.4) months (median of 29.9 months). During the follow-up, about one-quarter of the patients did not receive any LLT. Among treated patients, 89.5% received statins, and 10.5% received non-statin LLT. Less than half (47.6%) of the patients were adherent to the index treatment during the 12-month follow-up. Even in patients receiving combination therapy (statin + non-statin LLT), a sizable proportion (35.8%) showed increase in LDL-C over the follow-up period.
This retrospective study highlighted limited LDL-C monitoring in patients with ASCVD, and unmet need in terms of suboptimal utilization of non-stain LLTs, limited adherence to LLTs, and inadequate lipid control after treatment (among those with LDL-C measurements during the follow-up period) need to be addressed to improve outcomes in this patient cohort.